Gut restore & Colon Cleanse Diet
At LowFODMAPHelper.com, we make the Low FODMAP diet simple and effective for people with IBS, SIBO, Crohn’s disease, Colitis, Lactose Intolerance, and other digestive sensitivities. Our expert resources help you reduce symptoms, eat confidently, and manage your gut health every day.
🔎 What You’ll Find
- The Low FODMAP Diet for Beginners – step-by-step guidance to start your journey with confidence.
- Low FODMAP Diet Plan & FODMAP Diet for IBS – structured meal plans to manage IBS and other digestive issues.
- FODMAP Food List & Low FODMAP Foods – instantly see which foods are safe and which FODMAP foods to avoid.
- IBS-Friendly Foods & Recipes – enjoy delicious meals that support digestion without triggering symptoms.
- Low FODMAP Bread & Cooking Tips – make your favorite foods gut-friendly and satisfying.
- Low FODMAP Cookbook Recommendations – curated guides for easy, flavorful, and safe meals.
- Low FODMAP Food Calculator – our intuitive web app lets you quickly identify high and low FODMAP foods, explore alternatives, and modify recipes with confidence. Filter ingredients by FODMAP level, search by name, or browse categorized food groups to take control of your diet effortlessly.
Whether you’re just starting with the Low FODMAP diet or looking for advanced tips, LowFODMAPHelper.com is your trusted hub for IBS-friendly foods, meal planning, and symptom management.
Launch the Low FODMAP Food Calculator App in a separate window
Low FODMAP Food Calculator Key Features: 🔎 Smart search & filter for FODMAP levels, 📂 Browse by food category (fruits, grains, dairy, etc.),🥘 Get low-FODMAP recipe suggestions and swaps.
Understanding the Low FODMAP Diet
Too busy to read? Try the Low FODMAP Guide for Beginners in audio!
Related Free Tools
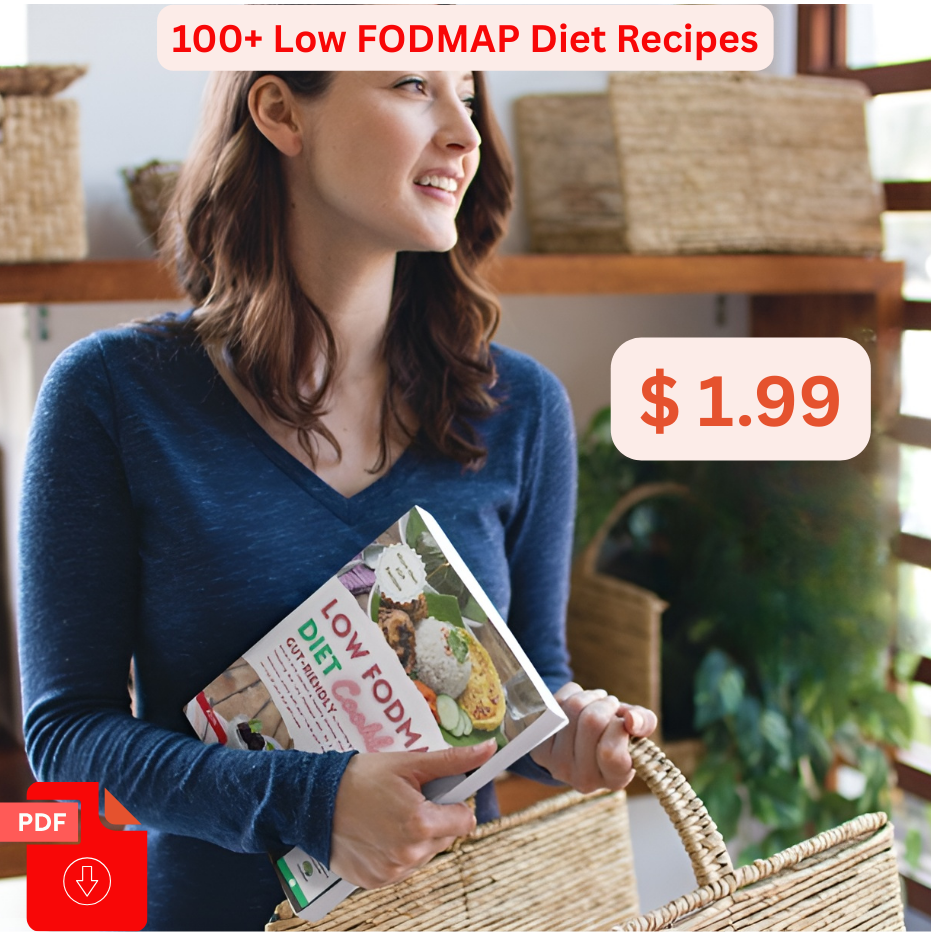
Low-Fodmap Diet Cookbook: Neutralizing Gut Distress Scientifically with IBS-Friendly Recipes
About this ebook
This comprehensive Low FODMAP Diet Cookbook is the perfect starting point. Designed to be simple and practical, it explains how to ease common IBS issues—like bloating, abdominal pain, constipation, and diarrhea—through smart dietary changes.
Inside, you’ll find Easy, delicious, and gut-friendly recipes to help you begin your Low FODMAP journey immediately
This book offers more than 100 meals recipes to help you restore balance to your digestive system and feel your best.
Enjoy our free downloads and take a step toward healthier and happier gut
Blog feed
Are Tomatoes Low FODMAP?Low FODMAP Diet
Is Low FODMAP High Protein?
Is Low FODMAP Good for SIBO?
Are Low FODMAP Foods Easier to Digest? A Guide to Gut-Friendly Eating
What Causes Bloating? Understanding the Root of That Uncomfortable Fullness
Rebuilding Your Gut: A Practical Guide to Healing Through Food, Recipes & Supplements
Frequently Asked Questions
Can a low-FODMAP diet cure IBS?
No, it doesn’t cure IBS, but it effectively manages symptoms in ~70% of people with IBS. It’s a tool to identify trigger foods, not a permanent solution. For long-term gut health, combine it with:
- Stress management (e.g., mindfulness, exercise).
- Adequate fiber (from low-FODMAP sources like oats).
- Probiotics (if tolerated).
Warning: Self-diagnosing or overly restricting FODMAPs can harm gut bacteria—consult a healthcare provider first.
Why do I feel worse when starting the low-FODMAP diet?
Possible reasons:
- Fiber changes: Sudden reduction in high-FODMAP fibers (like wheat or legumes) can cause constipation. Add low-FODMAP fiber (oats, chia seeds).
- Over-restriction: Cutting out too many foods can disrupt gut bacteria. Stick to the elimination phase for only 2–6 weeks.
- Hidden FODMAPs: Check labels for sneaky ingredients (e.g., garlic powder, inulin).
- Non-FODMAP triggers: Stress, caffeine, or fatty foods may also aggravate IBS.
Solution: Work with a dietitian to adjust the plan.
Are probiotics helpful on a low-FODMAP diet?
It depends:
Advice: Try a low-FODMAP probiotic (e.g., Align or Culturelle) after the elimination phase. Avoid probiotic yogurts with high-FODMAP additives.
Some probiotics (e.g., Bifidobacterium infantis) may improve IBS symptoms.
Others (especially prebiotics like inulin or FOS) can worsen bloating (they’re high-FODMAP).
How do I reintroduce FODMAPs properly?
Test one group at a time (e.g., fructose, then lactose, then sorbitol).
Start small: Eat a small amount (e.g., 1/4 cup mango for fructose) and wait 24 hours for symptoms.
Increase gradually if no reaction (e.g., 1/2 cup next day).
Keep a journal to track triggers.
Space tests 3 days apart to avoid confusion.
Example: Reintroduce garlic (fructans) separately from onions (also fructans), as tolerances may differ.