Wondering if tomatoes are low FODMAP? Learn safe serving sizes, tips, and check other foods with the Low FODMAP Calculator at LowFodmapHelper.com.
When following a Low FODMAP diet, one of the most common questions people ask is: “Are tomatoes low FODMAP?” The good news is that yes, tomatoes are generally considered low FODMAP in appropriate serving sizes. However, like many foods, portion size and variety matter. Let’s break it down.
Tomatoes and the Low FODMAP Diet
Fresh tomatoes are packed with vitamins, antioxidants, and gut-friendly nutrients. According to research:
- Common tomatoes (red, raw) are low FODMAP in servings of 1 medium tomato (about 100g).
- Cherry tomatoes are also low FODMAP at 75g (about 5 tomatoes).
- Roma and grape tomatoes are well tolerated in small servings.
- Canned tomatoes and tomato paste can become high FODMAP more quickly due to concentration, so portion control is key.
The takeaway: Tomatoes can safely be enjoyed on a Low FODMAP diet, as long as you stick to recommended serving sizes.
High FODMAP Risks with Tomatoes
Tomatoes themselves don’t contain high levels of FODMAP sugars, but problems can arise when:
- They are consumed in large amounts.
- They are used in sauces with onion, garlic, or other high FODMAP ingredients.
- Tomato paste or puree is eaten in large, concentrated servings.
Always check ingredients when buying packaged tomato products.
How to Enjoy Tomatoes on a Low FODMAP Diet
Here are a few safe ways to add tomatoes into your meals:
- Slice fresh tomatoes into salads.
- Roast cherry tomatoes with olive oil and herbs.
- Add Roma tomatoes to sandwiches or wraps.
- Use small amounts of tomato paste to flavor sauces.
Tomatoes are not only safe but also versatile and delicious when enjoyed mindfully.
Want to Check Other Foods?
If you’re wondering about other foods — like peppers, cucumbers, or eggplants — the easiest way is to use the Low FODMAP Food Calculator. It helps you instantly check if a food is safe, and even suggests low FODMAP alternatives.
Take Your Gut Health Further
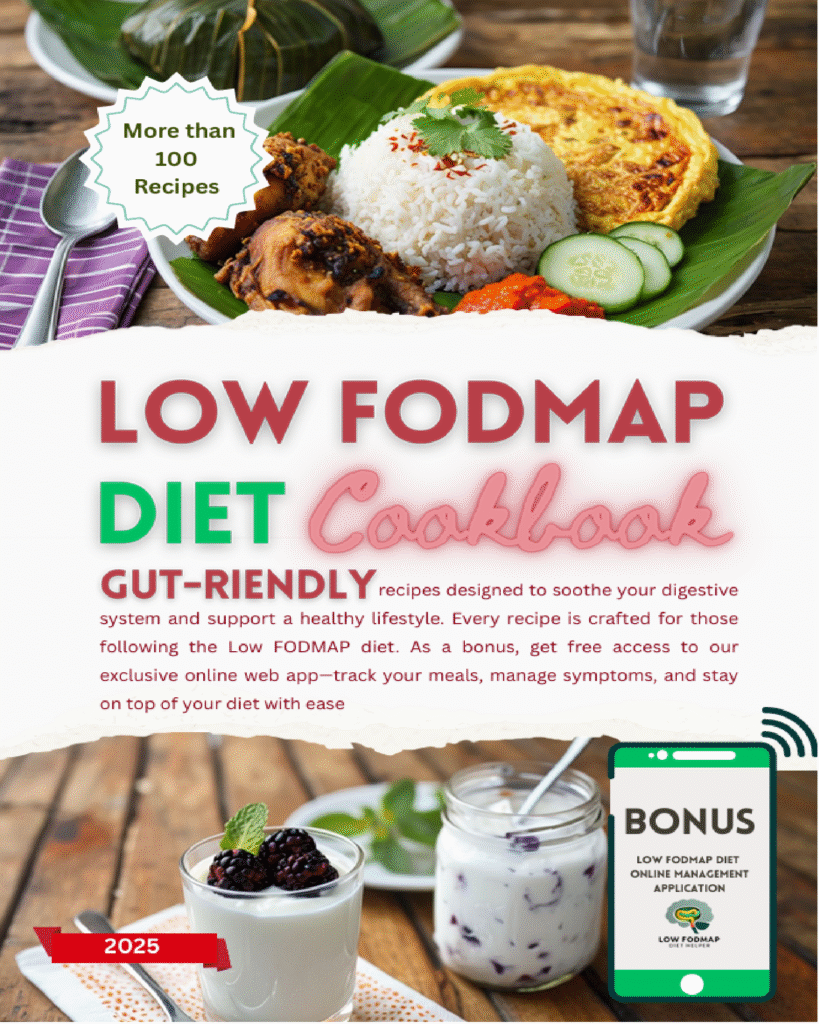
- Explore more delicious recipes with the Low FODMAP Diet Cookbook, designed to make your journey simple and tasty.
- For personalized guidance, visit LowFodmapHelper.com and access free resources, recipes, and food guides.
Final Thoughts
So, are tomatoes low FODMAP? Yes — when eaten in the right amounts, tomatoes are a safe and nutritious addition to your Low FODMAP diet. Stick to fresh or small portions of processed tomatoes, and avoid combining them with high FODMAP ingredients.
To make your diet easier, head over to LowFodmapHelper.com, check the Food Calculator, and grab your copy of the Low FODMAP Cookbook today.